“The National Diabetes Audit (NDA) is the largest annual clinical audit in the world”
We are incredibly lucky.
Unlike QOF, which was designed as a financial reward mechanism, the NDA integrates data from both primary and secondary care sources, making a comprehensive audit across the patient pathway.
This year’s audit upload period is between the 20th June to 29th July 2016.
In 2015, The NDA moved to an opt-in model to allow practices more control on what happens to their data. It requires about 20 minutes to upload the data in each practice once a year. Please don’t throw tomatoes at me. I know Practices are so overwhelmed that even 20 minutes feels like a big ask. Therefore, it is really important that CCG diabetes leads, communicate and support NDA participation.
I don’t think the NDA should be mandated but let me see if I can give you some important reasons to make the effort:
1)
The NDA data supports ensuring that your locally
defined diabetes pathway is sustaining and hopefully improving outcomes
2)
It helps to monitor the impact of any changes to
your diabetes model of care on patient outcomes
3)
Include participation in your local enhanced service
agreements to demonstrate the impact of investment on patient outcomes
4)
The NDA is used to support the Right Care Diabetes
pathway and Atlases of Variation
More information and lots of support for CCGs and Practices can be found on the NDA website.
This year there is one more reason to encourage and support participation.
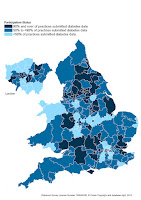
The CCG Improvement and Outcomes Framework was published on the 31st of March and the Technical Guidance was published last week. It clearly states that the source for the 2 diabetes indicators will be the National Diabetes Audit and that any CCG that has less than 25% of practice participation will be automatically placed on the lowest rating for diabetes. The performance against the 60 indicators will be published at the end of this month and will use the NDA data submitted last year (2014/15) so you can already see how your local CCG will fare. However, the performance for next year, 2017, will be collected in this month’s NDA upload period.
Have I persuaded you?